Get Involved: How We Can Increase Access to BPPV Treatment
By: Cheryl Wylie, MSc(PT) ∙ Estimated reading time: 5 minutes
By: Cheryl Wylie, MSc(PT) ∙ Estimated reading time: 5 minutes

Benign Paroxysmal Positional Vertigo Is More Common Than We Think
Benign Paroxysmal Positional Vertigo (BPPV), is a widespread and common condition, affecting 2.4% of the general population. Despite how common this condition is, only 8% of affected people receive effective treatment for it. Many patients get bounced around our healthcare system, seeing multiple physicians and incurring high medical fees before receiving just a diagnosis, let alone treatment.
This is a significant problem; however, it is a problem we can change.
Get to Know BPPV
BPPV is a condition of the inner ear and the most common cause of vertigo. Although its name is complex, it outlines really well what is going on:
- Benign: not life-threatening
- Paroxysmal: sudden brief spells
- Positional: symptoms are brought on by certain head movements or positions
- Vertigo: a sensation of spinning
The cause of this condition stems from tiny calcium particles called otoconia breaking free from their normal location in the otolith organs and migrating into the semicircular canals.
 Image source: Premier Neurology & Wellness Center
Image source: Premier Neurology & Wellness Center
The presence of the otoconia generates incorrect signals, triggering symptoms of dizziness, vertigo, imbalance, and nystagmus.
Therapist Role in BPPV
The role of the therapist is to maneuver the patient's head in specific orientations to move these otoconia out of the semicircular canal, where the body can then absorb the particles, resolving the patients’ symptoms.
BPPV and the Elderly
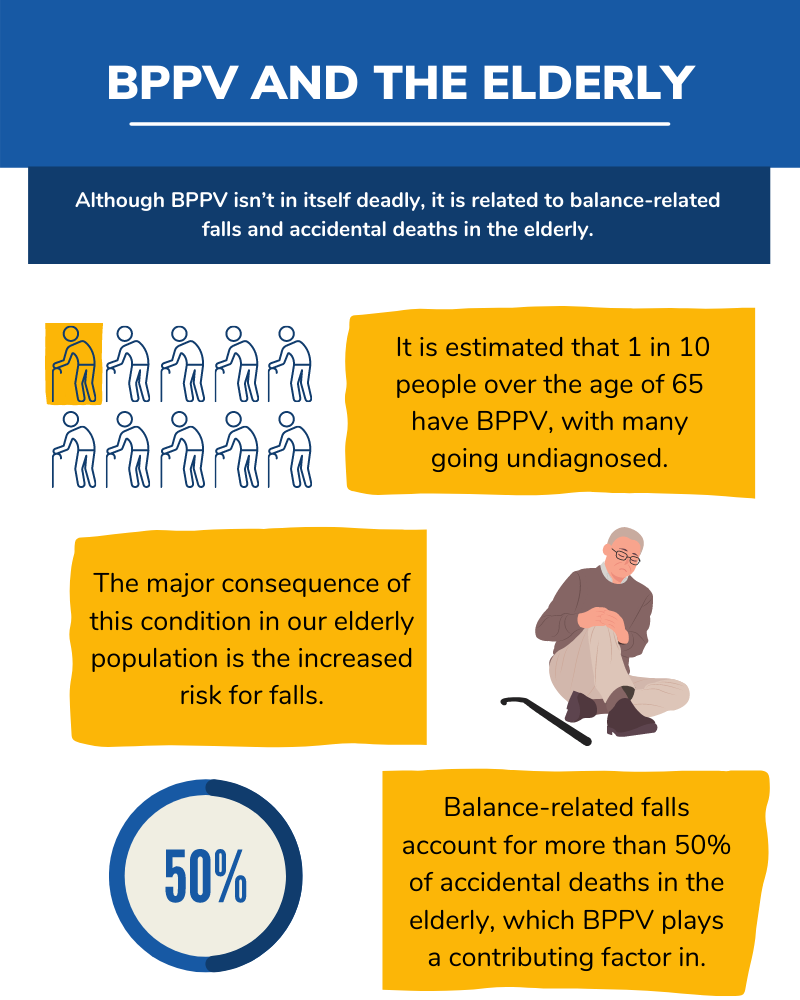
The prevalence of BPPV, as mentioned above, is quite high, especially in our older population.
Current Issues Surrounding BPPV
The issue surrounding BPPV at the moment is the time and cost of diagnosis.
In general, vestibular disorders are difficult to diagnose.
It is common for a patient to consult 4 or more physicians over a period of several years before receiving an accurate diagnosis, and BPPV is no exception to this, being the most prevalent of the vestibular conditions (VEDA).
Cost of BPPV
And the cost? It has been estimated that it costs nearly $2000 to arrive at a diagnosis of BPPV and that 86% of patients suffer some interruption in their daily activities and lost days at work because of BPPV.
Physiotherapy Education & BPPV
Improving these statistics lies in our hands as healthcare providers.
BPPV is a condition that is part of the vestibular system, a system that wasn’t taught for many years in physiotherapy programs. It has recently been included in the curriculum, but there are thousands of therapists out there who missed this opportunity to learn and understand this condition.
Course Goals
- The goal of this course and package is to set practitioners up for success in adding BPPV to their repertoire.
- It allows you to learn about the most common vestibular disorder, from simple to complex variations, in as little as 2 hours without having to dive into other aspects of vestibular therapy.
- Thinking back to that statistic we mentioned earlier that the average patient moves through 4 practitioners before receiving a diagnosis, improving practitioner awareness and confidence in treating BPPV is the first step in improving our patients' access to BPPV treatment.
Sample BPPV Treatment
To give you an example of BPPV Training, let’s take a look at the most common BPPV variation, which would be floating otoconia in the posterior semicircular canal.
This is referred to as posterior canalithiasis and is treated with the Epley Maneuver. Many therapists have heard of this maneuver, and likely you have even given it a try with your patients when you suspected BPPV as a cause of their vertigo.
The Epley maneuver is designed to move otoconia from the back of the posterior canal into the otolith organs through four simple steps.
Below is a video from Embodia’s BPPV Resource Package HEP of the Right Epley Maneuver:
Right Epley Maneuver
Tips on How to Succeed With the Epley Maneuver
Cheryl has completed this maneuver numerous times with her patients, and here is what she has learned to make it the most successful:
- Take your time. Traditional Epley Maneuver instructions recommend you hold each position waiting for your patient’s dizziness to stop, plus 30 seconds. Personally, I wait an additional 2 minutes after my patient’s dizziness has stopped. I do this because it often takes time for the otoconia to move within the canal, especially in our older population. By slowing down, I find I have increased success with fewer repetitions of the maneuver.
- Focus on the third position. There’s a reason why this position often causes the most dizziness in our patients, and that’s because it is the movement that really mobilizes the otoconia toward the exit of the canal. Make sure you roll your patients all the way onto their side and have them tuck their chin and point their nose down towards the bed.
- Tuck the chin! This is one of the most important tips to prevent complications such as converting the otoconia to a different canal. As just discussed, have your patient tuck their chin when you roll them onto their side, and then keep their chin tucked in the final movement when you sit them up. This ensures the otoconia move exactly where they are supposed to, and you get a quick resolution.
Hopefully, these tips help you the next time you do the Epley Maneuver with your patients.
Increasing Physiotherapy Awareness
Overall, BPPV is no longer a condition that has to be intimidating or reserved for management by vestibular physiotherapists. The more therapists that are aware of BPPV and know how to manage it, the more patients we will see get resolution in a timely manner, with a lower cost to the system and the patients themselves.
Learn More About How You Can Treat BPPV
This course and resource package, however, are just the start of Cheryl’s mission to increase access to BPPV Treatment.
In the past year, she has also developed an app called Healing Vertigo, which applies the logic flow of BPPV treatment along with the patient-focused videos into a simple resource tool that can be used by anyone, including patients themselves.
Let's improve BPPV outcomes together.
Resources:
- von Brevern M, Radtke A, Lezius F, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. Journal of Neurology, Neurosurgery and Psychiatry. 2006; 78(7):710–715. DOI: 10.1136/jnnp.2006.100420
- Oghalai JS, Manolidis S, Barth JL, Stewart MG, Jenkins HA. Unrecognized benign paroxysmal positional vertigo in elderly patients. Otolaryngol Head Neck Surg. 2000 May; 122(5):630-4. DOI: 10.1067/mhn.2000.105415. PMID: 10793337
- Agrawal Y, Ward BK, Minor LB. Vestibular dysfunction: prevalence, impact and need for targeted treatment. J Vestib Res 2013; 23:113–7. 10.3233/VES-130498
- Bhattacharyya N, Gubbels SP, Schwartz SR, Edlow JA, El-Kashlan H, Fife T, Holmberg JM, Mahoney K, Hollingsworth DB, Roberts R, Seidman MD, Steiner RW, Do BT, Voelker CC, Waguespack RW, Corrigan MD. Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo (Update). Otolaryngol Head Neck Surg. 2017 Mar; 156(3_suppl): S1-S47. DOI: 10.1177/0194599816689667. PMID: 28248609
---
Blog editor: Nataliya Zlotnikov, HBSc, MSc
Last update: 16 December 2025

MSc(PT), Vestibular Physiotherapist, Co-Founder of Healing Vertigo
Cheryl Wylie is a registered physiotherapist, receiving her Masters of Science in Physiotherapy from McMaster University in 2010. Prior to this she completed her Honours Bachelor of Science degree in Kinesiology from the University of Waterloo. She continued her education and completed with success the Vestibular Rehabilitation Competency-Based Course in Atlanta, GA hosted by Emory University and the American Physical Therapy Association. Since then, she has taken ongoing courses with a focus on vestibular and concussion rehabilitation, as well as shared her knowledge through in-services and lectures both locally and abroad.
Cheryl is the owner of Healing Vertigo, a focused vestibular physiotherapy practice in Hamilton, ON. Under the same name, she has also developed an App aimed to increase access to BPPV treatment for both patients and practitioners.